Introduction
In light of the tragic consequences of any type of disaster, it is not surprising to find an abundance of recommendations, guidelines or instructions on how to prevent, prepare or respond to such events.
While each of these pieces of literature is valuable in its own right by contributing to the safety and well-being of those involved, the EU-funded research project “PsyCris” (PSYchosocial support in CRISis management, SEC-2012.4.1-2 SEC-2012.4.3-1, GA. No. 312395), responded to the need to address aspects of psychosocial support for those in charge, namely the disaster management.
When considering all phases and aspects in which the disaster management is involved, it becomes apparent that psychosocial support is competing against numerous other responsibilities of often greater urgency. Yet, these complex tasks depend on the ability of the disaster management to maintain their professionalism, which in turn may depend on their (psychological) health. Thus, psychosocial support becomes particularly important in light of potentially costly long-term effects not only across the affected population, but also the disaster management itself.
This set of recommendations is based on and needs to be understood in conjunction with existing (European) standards, guidelines and recommendations on psychosocial support and mental health in disaster settings. While similar documents already exist, our recommendations aim to complement former suggestions by providing a specific framework of psychosocial aspects that focusses on strategic/functional features to prepare, implement and coordinate adequate psychosocial support in regards to the responsibilities of disaster managers.
Alongside these recommendations, PsyCris has developed an online platform, which may be used in conjunction with these recommendations. While the platform as well as these recommendations may be used independently of each other, their joint consultation is encouraged, especially for the purpose of deriving concrete actions via exchanges with peers and other professionals. Like the online platform, these recommendations have been developed considering the wider EU context and are based on minimum standards to facilitate cross-border psychosocial support.
The individual recommendations do not appear in any particular order. Each phase or sub-section can be read independently of each other, which means that certain aspects may be repeated, whereas others may be modified or changed.
For a brief tutorial on how to navigate this application, please click here.
You may also download a text version of the pssmgmt.de application, which contains reference tags for each individual item on the webpage. This version may help you referring to specific items when discussing the recommendations with others.
Purpose
While this set of recommendations might be an educating source of information for anybody interested in the topic, it has been developed with a particular focus on those involved in disaster management. The implementation and coordination of formal response and recovery measures (incl. psychosocial support) generally are assumed to fall within the strategic responsibilities of the disaster management and remain relevant long after the acute emergency responses. The respective operationalisation within existing support structures for potentially affected groups is typically available through specially trained units or response agencies. While the strategic implementation as well as the coordination of these support measures for all affected groups needs to be considered by the disaster management, measures for their own well-being are just as crucial. That is to say that psychosocial support needs to be considered not only by, but also for the disaster management, in order for the affected population to benefit.
Apart from their practical value, these recommendations also intend to support the continuous process of reflexion concerning the promotion and protection of public health measures and regulations on a national and European level. The presented aspects aspire to support those involved in disaster management (and beyond) to be at their personal best, stay healthy and add to their continuous efforts to improve responses to disasters.
However, this set of recommendations does neither offer specific approaches depending on particular disaster scenarios nor should it be understood as a contingency plan given that each incident contains unique elements that call for customized solutions. Instead, these recommendations provide the framework for and encourage the development of situation-specific, people-centred solutions within a pluralistic European environment. Thus, a focus is placed on strategic or functional aspects of psychosocial support. Since each disaster situation requires thoughtful implementations of existing plans and procedures, so does psychosocial support. Hence, this set of recommendations aspires to be applicable across disasters, populations, regions, cultures, legislations, etc. by means of generalizable aspects. These can either be adapted to the specifics of the particular situation or regional circumstances and might call for improvisation. Please note that these recommendations do not provide checklist-like steps. Instead, general best practice principles are suggested that need to be tailored to the specific disaster situation.
Definitions
Disaster
This set of recommendations focuses primarily on incidents, which are generally referred to as a disaster or crisis. Such situations are also described as major incidents and sometimes mass casualty incidents or mass emergencies. These events are usually distinguishing between either natural disasters (earthquakes, floods, etc.) or human-made disasters (technical accidents, terror attacks, etc.). Since the defining features are highly circumstantial, the following aspects may be of help describing such events:
Significance/Impact of the incident
Disasters usually have a high significance/impact in terms of damage and number of affected people. However, the significance/impact of an incident varies according to its nature and circumstances (e.g. school-shooting vs. earthquake), thus rendering the respective features to be relative in comparison. Variables such as individual/collective capacities to adapt and available help may moderate the impact of such events.
Character/dimension of the incident
Disasters are often outweighing available resources and exceed the capacities (social mechanisms, financial, human resources, etc.) of the affected communities. In addition, such events are often highly unforeseeable, uncontrollable and unpredictable. However, the responses (from preparation to longer-term efforts and consequential improvements) usually differ significantly between events with a sudden/rapid onset (e.g. terror attack) or a slower onset (e.g. flood).
Extent of (potential) damage
Generally, larger extents of structural damage (e.g. material, financial, geographical, etc.) of damage are helpful indicators to describe such incidents. However, structural damage may also severely compromise societal functions, which may exceed the structural damage. Quantitative as well as qualitative parameters need to be considered when assessing the magnitude of the damage and the significance of the event. Geographic settings also need to be considered (e.g. central disasters, like floods where an entire community is affected vs. peripheral disasters like an aircraft accident in an unpopulated area, where individual survivors return to respective geographic homes).
Number of affected people
Higher numbers of affected people (both directly and indirectly) usually mean more damage. However, the significance of the incident serves as an important indicator when determining quantities (e.g. four casualties in a train accident vs. four casualties in a terror attack). Disruption (sudden-/ or slow-onset) of social structures may also have significant effects on the population.
For the purpose of these recommendations, a disaster may be discribed as a severe disruption of societal functions and structures that exceeds the readily available resources of the affected communtiy. Concerning psychosocial support, it needs to be noted that individuals or groups may be affected to different degrees, at different times and rates. Thus, their needs as well as the corresponding response and recovery measures may also differ significantly from each other.
Strategic and tactical planning
For the purpose of this set of recommendations, the term strategic will refer to measures that consider the broader concepts rather than the specific steps, thus forming the top decision-making level of crisis management. Hence, strategic planning would refer to the overarching aims of disaster management and describes broad, general and sometimes abstract (non-specific) aspects of what needs to be achieved. The term tactical will refer to the operationalisation of strategic planning and usually includes the definition of concrete objectives. Strategic and tactical planning requires close cooperation and information exchange. The lowest level of decision-making in disaster management will be referred to as operational and includes less planning and focuses on the execution of strategic and tactical plans and the achievement of the respective objectives.
Prevention and intervention
The term intervention is often used to describe measures intended to actively alter developments or circumstances to promote health and/or resilience. However this set of recommendations follows the salutogenic notion, meaning that such actions can be integrated into the broader framework of prevention. Drawing on the salutogenic terminology of primary, secondary, and tertiary prevention such preventive actions can be grouped either chronologically and/or functionally. To avoid misunderstandings with these terms originally developed for medical and psychological treatments, three modified terms are introduced in the following. Based on an approach of overlapping disaster phases, these new terms attempt to resonate with the cyclical character of the presented disaster phases. Thus, the concepts of intervention and prevention will be described by at least one of the following distinctions:
Continuous prevention
Continuous prevention refers to all measures aiming to avoid potentially harmful situations as well as prepare for potential emergencies. It is identical to primary prevention in a medical/psychological sense, but may include administrative and technical details, too. Thus continuous prevention is a constant effort prior to an incident (e.g. preparedness and planning) as well as following an event (e.g. mitigation, improvements).
Intermediate prevention
Intermediate prevention refers to all immediate measures (e.g. safety, relief) and includes secondary prevention in a medical/psychological sense (e.g. acute care, psychological first aid). It is aiming to respond to potentially harmful situations and to prevent or minimise further destructive consequences as a result of an incident. “Intermediate” describes the aspect that this form of prevention is neither continuous nor extending over long periods of time.
Extended prevention
Extended prevention refers to all post-immediate measures aiming to respond to, recover from and limit potentially harmful consequences as well as preclude subsequent damage as a result of an incident often extending over longer periods of time (e.g. follow-up care, longer-term support). While it includes elements of tertiary prevention, a focus is placed on follow-up and low-threshold transitions to receive medical/psychological care from respective providers. It may also include administrative and technical details that go along the offered support.
It needs to be noted that primary (e.g. acute, on-site), secondary (e.g. hospitals, public healthcare) and tertiary (e.g. health specialists, psychotherapist) care refer to different levels of medical/mental forms of treatment.
Psychosocial support
In the context of disasters and major incidents, psychosocial support (PSS) includes the short-, mid- and long-term provision of continuous, intermediate and extended prevention. Among the general objectives are early recognition of stress-related consequences after major incidents as well as the provision of adequate, needs-based support (e.g. psychological, social, structural, etc.) for individuals and groups of directly or indirectly affected people as well as rescue/emergency personnel (e.g. psychological first aid, processing of experiences, appropriate help to access treatment for trauma- and stress-related disorders). Hence knowledge of regional and/or national structures (formal and informal) and close collaboration with existing regional networks is considered advantageous. Psychosocial support comprises the preparation, provision, implementation, and coordination of all offered strategies and intervention methods that are geared to maintain or reach a normative level of pre-event functioning and aim to promote public health and foster resilience/collective-efficacy. This is done in close cooperation with respective psychosocial operatives, medical units and existing community structures as well as by forming secondary and tertiary (health-)care networks. In that regard, psychosocial support is not considered a consequence of a demand, but a task automatically generated by the disaster itself. That is to say, at least in the sense of screening the potential need for such support. Sufficient and adequate psychosocial support can significantly contribute to: damage limitation, (re-)establishing order and a sense of safety, fostering resilience and self-efficient functioning of individuals and communities as well as the prevention of often costly longer-term effects on health. Thus, psychosocial support is usually needed to different degrees throughout all phases associated with a major incident or disaster.
Potentially affected population
Affected persons are all surviving individuals who have been somehow involved in a disaster situation and are influenced (e.g. develop medical/mental problems) as a result of it. They can be further subdivided into directly and indirectly affected people.
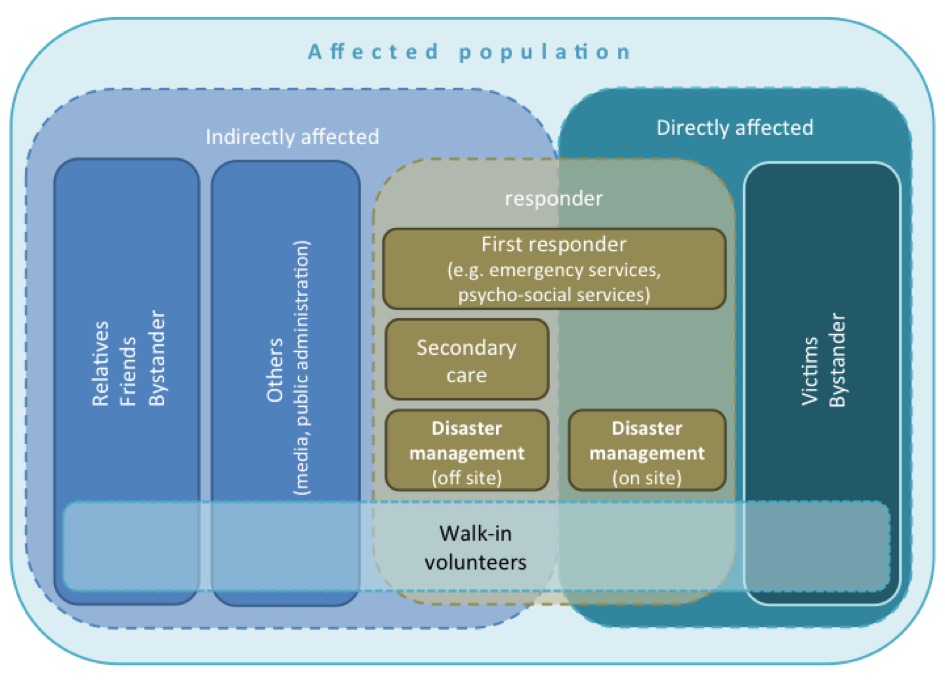
Directly affected persons are those involved first-hand, for instance as victims of and/or witnesses to the event(s). This is usually characterised by experiences of or exposure to threat to physical integrity or serious injury, danger of death and other physically and mentally disturbing or harmful experiences.
Indirectly affected persons on the other hand are not involved first-hand. They may be affected via their relationship to a directly affected person, direct contact with a victim, or explicitly disturbing knowledge of the event, etc.
Both groups may include civilians as well as responders as well as certain groups with special needs that have to be considered in regards to psychosocial support. For the purpose of these recommendations, such special needs cover all groups that are known to be particularly vulnerable (e.g. children / families, young, elderly or disabled people, marginalised groups, people with pre-existing medical/mental conditions) or whose value system may be accompanied by respective needs (e.g. faith-related customs and restrictions, cultural boundaries, value-related interests). In order to be able to provide psychosocial support appropriately, such needs have to be considered as early as possible and usually require additional planning and resources.
Everyone involved in a disaster situation may be directly or indirectly affected and present responders with all kinds of needs that may become apparent throughout all phases to different degrees. The respective needs are likely to differ across groups and phases. That is to say that relief or recovery efforts may vary in time and duration for different groups. Consequentially, the disaster phases may overlap and different groups may experience to be in different phases at different times. Adequate (psychosocial) support depends on the coordination of needed and available responses by the disaster management under these given circumstances of the specific disaster situation.
Disaster management (strategic/tactical)
The main task of the disaster management is the strategic coordination of actions and missions following a major incident. They are strategic (golden) and tactical (silver) commanders of responding institutions, public authorities, agencies for technical relief, or the military, etc., and are either permanent heads or members of a disaster management unit or can be nominated or appointed respectively. They are usually involved on at least one level of psychosocial support in light of their involvement in safeguarding, protection, rescue, dissemination of information, needs analysis, identification of people at risk, organization of psychosocial support, or follow-up care, to name a few. They have staff and decision-making responsibilities and belong to the middle and higher management. The disaster management team usually consists of at least one leader and a deputy. There may be other specific roles or responsibilities like "communication" or other specific support, which can be divided among additional members. One or more individuals may cover any roles/responsibilities. The disaster management is often supported by a technical assistance team. Disaster managers usually disengage towards the end of the non-emergency intervention phase or during the following post-incident phase, but may also be involved in later phases to different degrees. Regardless of the specific civil protection or disaster management focus, members of the disaster management may be stationed at the scene of the event (on-site) or be working out of an emergency control centre (off-site).
First responders/emergency personnel
First responders are professionals working on site, who react instantly after an alert. During disasters they are typically active in the emergency and emergency intervention phase. They are usually members of emergency agencies, such as the fire brigade, medical services, rapid deployment forces, or the police department. They are responsible for search and rescue, triage, and the protection and evacuation of the public. This includes providing medical, technical and psychological first aid for victims.
Psychosocial support personnel
Psychosocial support includes the short-, mid- and long-term provision of adequate support for individuals and groups of directly or indirectly affected people as well as rescue/emergency personnel and the disaster management. Thus, psychosocial support is ideally already represented within disaster management structures (cf. definition ‘Disaster Resilience Manager’). On- and off-site support may be provided through specialised formal/official agencies and structures as well as professional, but informal networks from within the affected communities. Personnel with psychosocial responsibilities are often called psychosocial support operatives/units.
Disaster Resilience Manager
The introduced title “Disaster Resilience Manager” has to be understood as a suggestion and not as an existing title. Although the appointment of a Disaster Resilience Manager is strongly suggested, the implementation of these recommendations does (should) not depend on such a position. As with the entire set of recommendations, the position of a ‘Disaster Resilience Manager’ needs to be customised and tailored towards the specific situation. One particular responsibility of the general disaster management is to implement, coordinate and manage the provision of psychosocial support for all affected persons. For that purpose, the disaster management unit may include a specially trained expert for psychosocial prevention, support and aftercare, who strategically operates within existing plans. Under the assumption that the disaster management unit may not find the time or resources to adequately attend to matters pertaining to psychosocial support, the main responsibilities of these “Disaster Resilience Managers” (DRM) would be to implement and coordinate all offered strategies and interventions throughout all phases (short-, mid- and long-term provision of psychosocial support) associated with a major incident or disaster. This includes all relevant aspects of continuous, intermediate and extended prevention efforts offered to civilians and responders alike, which need to be considered by the disaster management. In addition, they would also function as special advisors concerning psychosocial support for the disaster management itself, which not only includes support during the relief and recovery phases, but also the preparation phase (e.g. development process of disaster response plans, resilience building measures, etc.). Like the general disaster managers, these Disaster Resilience Managers work ideally as an equal member within the disaster management unit; thus ensuring continuous representation of psychosocial support within existing structures. That means that psychosocial command structures, staff and decision-making responsibility are ideally analogous to the respective disaster management structures.
In order for the Disaster Resilience Manager to be adequately equipped, specific training would be required. Apart from basic education in psychology/psychotraumatology or equivalent disciplines, explicit training in psychosocial support for all phases is recommended. This could include specific disaster management training (incl. exposure to and familiarisation/experience with existing structures and plans) and organisational management and media training, while preferably having specific knowledge of the affected communities.
A note on terminology: Although the exact terminology used to describe the position of the Disaster Resilience Manager may be adapted to the respective existing structures, the rationale for the term is that those responsible to manage/coordinate responses following a disaster are widely referred to as 'disaster managers' (in English at least). Due to the strategic involvement from preparedness to longer-term support encompassing all relevant aspects of continuous, intermediate and extended prevention, the notion of fostering resilience may be seen as a central attribute of the position of the Disaster Resilience Manager. Thus, aligning the title with comparable roles, the 'Disaster Resilience Manager' may easily be introduced as a personified representation of psychosocial support within existing disaster management structures.
Description of disaster phases
For the purpose of illuminating psychosocial support considered by as well as for the disaster management, the course of a disaster is broken down according to functional descriptions of phases. These phases attempt to cover all stages in a cyclical motion and offer a descriptive framework from a strategic perspective while already considering psychosocial aspects. The overview in the figure below shows the proposed disaster phases (grey circle) in relation to other common phase descriptions (inner circle) as well as the abovementioned concepts of prevention (outer circle). It has to be noted that the duration of each phase depends largely on the specific incident and the suggested time-frames can only be understood as an indication. Since individuals or groups may be affected to different degrees, at different times and rates, it also needs to be taken into account that the transitions between them can be very fluent and that certain features of one phase may occur in parallel to or overlap with other phases and even progress asynchronously for different groups.
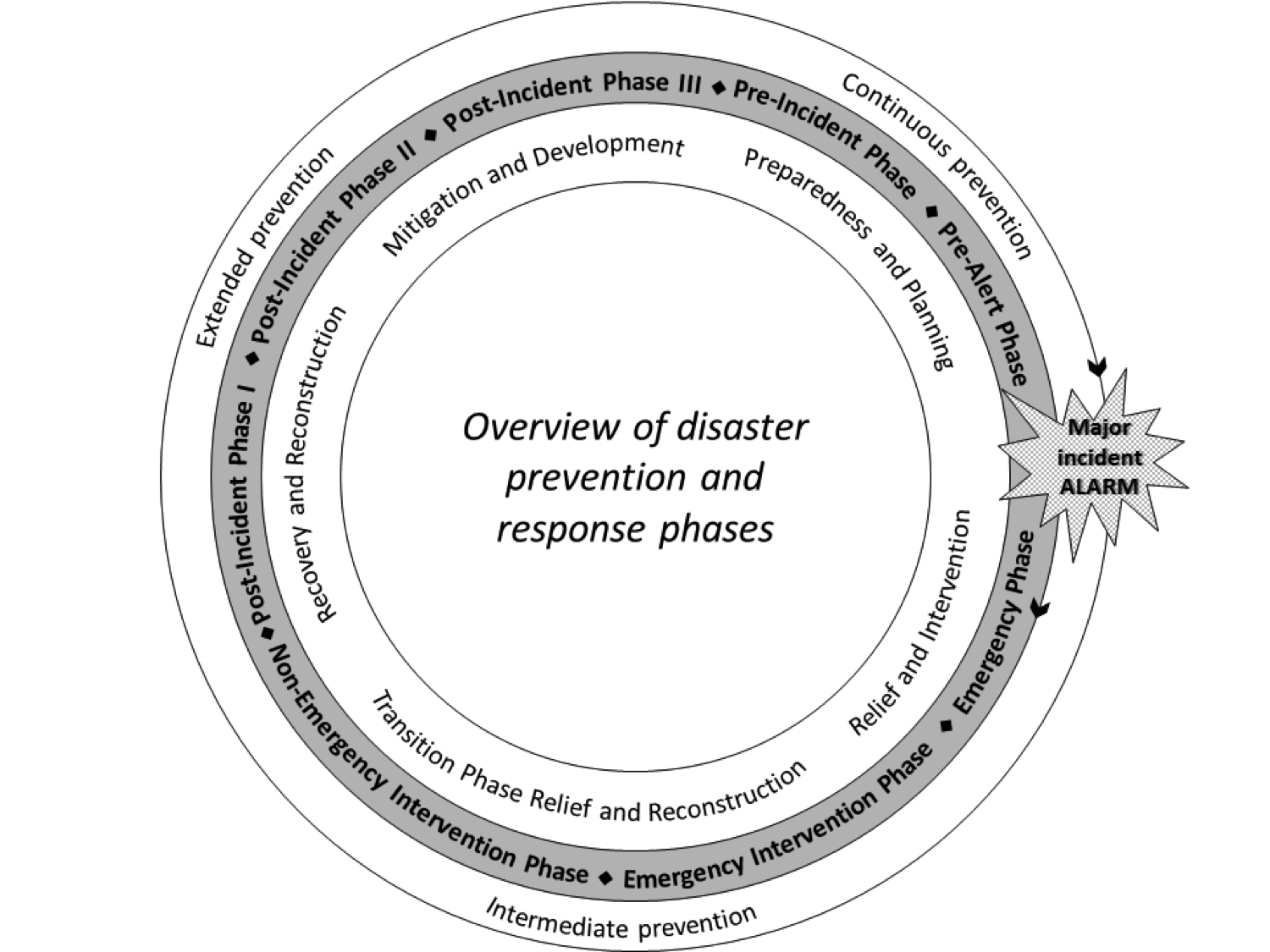
Each phase will briefly be described in the following:
Pre-incident phase
Every effort to prevent potentially harmful situations as well as prepare for potential emergencies or disasters (i.e. continuous prevention) could be seen as a part of this phase. This also includes all efforts intended to improve the functional status compared to the levels before the last incident occurred.
On a societal level this may include: information, education, implementation and improvement of safety measures, preventive measures of protection (technical, social, cultural, etc.) and generally everything that develops and strengthens collective-/ and self-efficacy in case of a disasters. Respective policies or plans may be created or amended where necessary.
On a responder level this may include: trainings, exercises, education, technical preparation and tests, service assessments, development and improvement of response/action/contingency plans (incl. equipment, infrastructure, supply chains, human resources, etc.). This includes all agencies that are possibly involved in disaster responses and post-incident missions (and secondarily the general public).
Other involved groups may be: insurance companies, political entities, scientific/research institutions, engineers or software developers, local initiatives, community/spiritual leaders, etc.
Time-frame: The pre-incident phase is on-going whenever none of the other disaster phase descriptions applies. It may also already commence in parallel to later disaster phases.
Pre-alert phase
The goal is to prevent/avert possible risks or dangers or prepare for a potential incident. This usually includes gathering knowledge about consequential/additional risks (e.g. weather, terror warnings) and potential infrastructure limitations as well as the activation of respective existing alert/action plans and respectively needed agencies. If available, the potential situation may be graded in a standardised way. Additionally, adequate provision of information to responders and the public may be needed. For optimal preparation it may be important to verify available/adequate resources (incl. manpower) and obtain preliminary clarification of possible causes. However, preparations are only possible to a certain extent and specific needs may still be unclear. This phase may not exist in case of rapid/sudden onset disasters.
Key groups that may be involved in this phase are: emergency personnel, police, civil protection management, technical assistance, politicians, psychosocial support, local initiatives, press/media/social media, or military.
Time-frame: The pre-alert phase starts whenever threats or concrete indicators for potential danger emerge. This may last from minutes to several days (i.e. slow vs. sudden onset). It needs to be noted that this phase continues even after the onset of an incident, as further incidents are possible and lasts until the possibility of such further (second onset) incidents is very unlikely. Hence this phase may overlap with the following phases, sometimes extending into the emergency-intervention phase.
Emergency phase
The goal is to scale the dimension of the incident/damage and to implement respective safety measures. These on-going efforts usually encompass the prevention of further damage and chaos, creation of order, activation of emergency plans and all needed resources as well as setting up a communication network and emergency specific infrastructures (e.g. organization of access/routes to needed supplies, and facilities/hospitals). Initial responses also include preparations for possible evacuations before or during further damage, acute search and rescue and triage. This phase may be characterized by breakdowns of critical infra- and social structures and essential services (including the possibility of limited access for responding services) and potential lack/loss of access to supplies for basic needs. The dimension of the incident might still be unclear (i.e. lack of information) and be very chaotic. Clarification of possible causes is usually underway. Current needs are not (adequately) met and further needs may still arise (including a second incident). Hence, the mortality/morbidity rates might be very high. Responding agencies are consequently exposed to all possible risks/dangers. Among the affected population may be directly affected civilians, bystanders and first responders and indirectly affected people.
Key groups that may be involved in this phase are civil protection/disaster management, search and rescue/emergency services, technical support, psychosocial support coordination, and press/media/social media.
Time-frame: The emergency phase starts with the official alarm or once an incident requiring emergency responses has been verified. The situation cannot be reversed at this time and might have gone beyond control. The phase lasts until all search and rescue/emergency services are at full strength according to the emergency plans or until the incident zone is secure. This may last from minutes/hours to days and usually overlaps to a large extent with the following phases.
Emergency intervention phase
The goal is to continue with search and rescue, prevent further harm/damage and meet acute needs (e.g. medical first aid/acute assistance). This also includes evacuations and transfers to nearby facilities/hospitals, providing psychological first aid and starting to recover dead bodies. Missing people lists are prepared, however disaster victim identification (DVI) usually has not yet begun. The situation may still be unstable, or even precarious. Breakdowns of critical structures and essential services might be on-going and access to the area may still be limited. Clarification of possible causes is usually still on-going. The coordination of involved agencies and the involvement of walk-in volunteers may create additional challenges. The affected population may include directly involved civilians, bystanders, emergency personnel, police, disaster managers and indirectly affected people (e.g. spectators, relatives).
Key groups that may be involved in this phase are civil protection/disaster management, search and rescue/emergency services, medical and psychological first aid units, technical support, evacuation teams, police (incl. forensic teams), press/media/social media and politicians.
Time-frame: The emergency intervention phase begins as soon as response units/operatives are in a position to respond and ends when the chance of rescuing victims alive is exhausted and the possibility of further (second onset) incidents is unlikely (i.e. the incident zone is secure). Please note that the transition between the emergency and the emergency intervention phase is often fluid and difficult to differentiate (especially with slow onset disasters). This phase may last from hours to weeks.
Non-emergency intervention phase
The goal is to further stabilize the situation, prevent further harm/damage and provide on-going medical assistance. The recovery of dead bodies may still be on-going. All psychosocial services are available (e.g. psychological first aid, psychosocial assistance, hotline/website, social/financial/legal/resettlement support) as well as facilitating transitions to regular (long-term) facilities (e.g. mental health facilities, in-/out-patient treatment, rehabilitation centres). The search and rescue workers usually disengage during this phase. Cleaning up of the site has begun and vital infrastructures are being restored. The situation is increasingly more stable and civilians may start to (re-)establish (informal/transitional) structures and routines to create order. The coordination of involved agencies and the involvement of walk-in volunteers may still be challenging. If necessary an in-depth analysis of causes may be commenced during this phase. Funds for on-going and longer-term efforts may need to be clarified. The affected population may include directly affected civilians, bystanders, emergency personnel, walk-in volunteers, police, disaster managers, non-emergency responders and indirectly affected people (e.g. spectators, relatives).
Key groups that may be involved in this phase are civil protection/disaster management, disaster response units, police, medical units, psychosocial services, secondary healthcare services, forensic teams, disaster victim identification units, local initiatives, press/media/social media, community/spiritual leaders, politicians.
Time-frame: The non-emergency intervention phase starts when the zone is secure/threat is contained and/or the chance of rescuing victims alive is exhausted and all survivors are brought to safety (e.g. evacuated, in hospitals, in shelters). It ends when the disaster site is accessible to civilians and all basic infrastructures are restored. This phase may last from days to months and usually overlaps with the following phases.
Post-incident phase I
The goal is to further stabilize the situation and provide on-going medical and psychosocial support (usually off-site) as well as maintaining good transitions to secondary and tertiary healthcare/long-term support. The identification of dead bodies is complete. Cleaning up of the site may still be on-going. Immediate psychosocial support for emergency services has been completed and all acute services have retired. However, supportive aftercare services (e.g. hotlines, proactive follow-up of potentially affected, contact points/coordination centres, funerals, financial/legal/resettlement assistance, rebuilding, etc.) and coordination of volunteer engagement may still be necessary. Further analysis of causes may be on-going. Funds for on-going and longer-term efforts may need to be clarified. In addition, initial evaluations of the acute response may commence. The affected population comprises all that were potentially affected by the disaster up to this point (directly or indirectly) and may also include those who are recently involved (e.g. secondary support, cleaning up, etc.)
Key groups that may be involved in this phase are civil protection management, technical support, secondary and tertiary healthcare, psychosocial services, community services, community/spiritual leaders, local initiatives, politicians and press/media/social media.
Time-frame: The post-incident phase I starts when vital infrastructures are restored and access to most main areas can be permitted without restrictions. Civilians are in a position to start (re-)adjusting to daily life/normal routines. It ends when stable solutions for longer-term support are established. This phase may last from days to sometimes over a year.
Post-incident phase II
The goal is to further stabilize the situation, to continue cleaning up and to implement or uphold longer-term (community) services in residency (e.g. psychosocial assistance, hotline/website, financial advice, restoration services, educational work). The dependency on most intermediate aid services has ended. The analysis of causes is usually complete. Technical, structural, educational, social, and other preventive measures derived from the incident may have already begun. This may affect the establishment of permanent solutions (often different from the original ones). However, the evaluation of involved services and collection of lessons learned may still be on-going. Funding for longer-term efforts may need to be clarified. The affected population comprises all that were potentially affected by the disaster up to this point (directly or indirectly) often with signs of ongoing distress.
Key groups that may be involved in this phase are coordinating bodies, secondary and tertiary healthcare, psychosocial and community services, community/spiritual leader, local initiatives, politicians and press/media/social media.
Time-frame: The post-incident phase II starts when stable solutions for longer-term support are established. It ends when all (infra-)structures and societal functions have at least reached pre-event status. This phase often already links with the pre-incident phase in a cyclical motion and may last from weeks to years.
Post-incident phase III
The goal is on-going prevention and stabilisation through maintaining specific longer-term/permanent community services, if necessary (i.e. continuous prevention). This includes educational and social measures as well as healthcare and on-demand services and assistance. Most technical/structural improvements derived from the incident are completed and link with the pre-incident phase in a cyclical motion. Funding may need to be clarified. Memorial events/remembrance days may be repeated over a very long period. Among the affected population may be those with chronic symptoms/condition, including directly affected people and indirectly affected people.
Key groups that may be involved are coordinating bodies, secondary and tertiary healthcare, psychosocial and community services, local initiatives, community/spiritual leaders and politicians.
Time-frame: The post-incident phase III starts when all (infra-)structures are restored, everything is cleaned-up and most long-term services are hardly needed. This phase usually runs in parallel to the pre-incident phase. However, it describes measures and services still associated with the original event. It may last from months to years.
Limitations and additional material
The presented set of recommendations is by no means exhaustive and requires adaptation to the given circumstances, such as: type and duration of the disaster, available resources (human, material, etc.), time, value systems / culture (incl. spiritual beliefs and rituals), etc. As stated before all efforts to provide psychosocial support from and for the disaster management need to be customised and tailored towards the specific situation.
Such a process of deriving concrete actions from the presented strategic/functional aspects would require careful assessment and planning prior to an incident and under consideration of given resources and circumstances.
For further details regarding the development process of these recommendations, please contact the author.
Credits
Author: Jona Meyer on behalf of the guideline development group at Ludwig-Maximilians-Universität München, and in close cooperation with our project partners.
We would like to specially acknowledge and express our gratitude to the following colleagues and external scientific advisors, without whom this document would not have been possible:
Dr. Maria Hagl (Germany), Marc Stein (Luxembourg), Guy Weis (Luxembourg), Professor Dr. Lars Weisæth (Norway).
We would like to specially recognize and thank the following members of the European Federation for Psychologists' Assosiations (EFPA) Standing Committee for Crisis and Disaster Psychology, who thoroughly evaluated these recommendations in light of the current state-of-the-art:
Lucia Formenti (Italy), Nathalie Garcia Manitz (Andorra), Eva Håkanson (Sweden), Eva Münker-Kramer (Austria), Dr. Julia Richter (Hungary), Magda Rooze (Netherlands), Dr. Salli Saari (Finland), Márcio Simão Pereira (Portugal), Marc Stein (Luxembourg), Dr. Dominique Szepielak (France), and Professor Dr. William Yule (United Kingdom).
We also would like to acknowledge the kind and tireless collaboration of our project partners:
Amuta LeYeladim beSikun - Cohen-Harris Resilience Center for Trauma and Disaster Intervention (CHC, Israel), Colegio Oficial de Psicólogos de Andalucía Oriental (COPAO, Spain), Kitokie projektai (KKP, Lithuania), Private Universität für Gesundheitswissenschaften, Medizinische Informatik und Technik (UMIT, Austria), Protection Civile Luxembourg Groupe de Support Psychologique (GSP, Luxembourg), Universidad de Granada (UGR, Spain).
Last, but not least, we would also like to thank Attila Sirman Digital Consulting (Germany) for their support in developing this online version.
An earlier version of these recommendations was submitted to the Research Executive Agency (REA) at the European Commission in December 2014; and accepted in April 2015.